As many of you are aware, atypical myopathy is a deadly disease with devastating consequences for both the horse and the owner. Atypical myopathy in horses occurs when components, usually seeds or shoots, of the sycamore tree (Acer pseudoplatanus) are ingested. One of the features that makes atypical myopathy so fatal is the relatively tiny amount of toxin required to cause disease in horses. Sadly, once the toxin has been absorbed into the bloodstream, there isn’t much we can do. This post aims to explain the disease process behind sycamore toxicity and why we have seen an increase in cases in recent years.
Sycamore trees, Box Elder trees, and the unripe fruit of the Ackee tree all contain a naturally occurring protein called hypoglycin A. If a human ingests the unripe fruit of the Ackee tree, a clinical syndrome extremely similar to atypical myopathy called Jamaican vomiting sickness is caused. The Ackee tree is not indigenous to the UK, but there is a plant commonly found in this country that contains a very high concentration of this toxin – the sycamore tree.
When hypoglycin A enters the body, it is rapidly broken down to the active toxin methylene cyclopropyl acetic acid (MCPA). This toxin blocks one of the key enzymes involved in the conversion of fatty acids to usable cellular energy. This prevents cells from metabolising fatty acids and making new molecules of glucose. Think of fatty acids and glucose as petrol and diesel, and hypoglycin A as a blockage in the fuel tank. When the supply of fuel is cut off, cells must start using their “reserve fuel” called glycogen. Once this back up fuel is used up, the cells have no way of obtaining a fuel source and the cell’s engine begins to shut down. This is why there is a delay between toxin ingestion and the appearance of clinical signs.
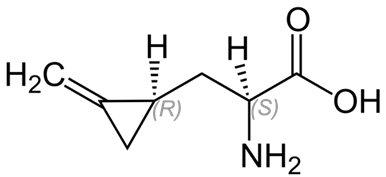
Figure 1: Hypoglycin A
The cells that run out of fuel first are the ones with the highest energy demands. One of the cells that work the hardest in a horse’s body are the muscle cells (myocytes). These muscle cells are the first victim of hypoglycin A toxicity, hence the name atypical (not typical) myo- (muscle) -pathy (disease). When the muscle cells begin to starve, signs such as sweating, muscle lethargy, muscle weakness, muscle fasciculations and tremors, colic signs, and dark coloured urine are seen. As the disease progresses, more and more cells begin to run out of fuel, resulting in worsening clinical signs. The deadliest feature of atypical myopathy is that the actions of hypoglycin A are irreversible. Once MCPA has blocked the cell’s fuel tank, there is no going back. The only hope is that the amount of hypoglycin A ingested was small enough that only some of the cells have a blocked fuel tank, and enough have been unaffected.
Recently, we have seen an sharp increase in atypical myopathy cases caused by an increase in the amount of hypoglycin A in the environment. The term “mast year” is used when a tree produces an abnormally high number of seeds. These seeds will subsequently go on to produce an abnormally high number of shoots. It is this phenomenon that has caused the higher-than-average number of atypical myopathy cases in recent years. Although the concentration of hypoglycin A in seeds and shoots varies dramatically, only a very small amount is needed to cut off the fuel supply to all the cells in a horse’s body. The only way to stop this devastating disease is to prevent horses from ingesting seeds and shoots containing hypoglycin A.
For further information regarding atypical myopathy, please click here. If you have any questions, please don’t hesitate to contact us on 07747 771 182.






